Fractures of the Jaw and Face
Patients who experience injury and fractures in the jaw and face area following accidents, sudden incidents, or conflicts should seek immediate attention from a specialized maxillofacial surgeon to determine the initial treatment plan as soon as possible and take necessary actions.
However, if a significant amount of time has passed since the occurrence of the incident, there is no need to worry. You can consult with our specialized maxillofacial surgeon for visits and therapeutic and cosmetic interventions.


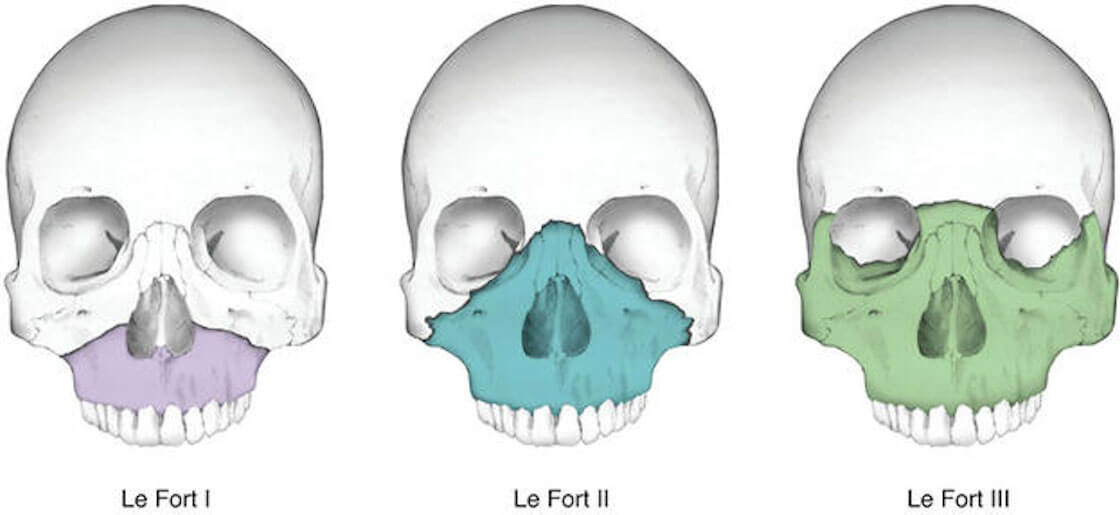
Upper Jaw Fractures
Fractures of the maxilla (upper jaw) can occur as a result of any type of incident, including accidents, conflicts, falls from heights, and so on. Fractures in the upper jaw are classified into three categories: LeFort I, LeFort II, and LeFort III.
These fractures are usually accompanied by tooth fractures, palate injuries, etc., which should be distinguished from bone fractures, and separate treatments for the teeth should be carried out. In this type of fracture, there is a possibility of damage to the upper lip, upper lip laceration, and penetration of foreign bodies into the oral mucosa and soft tissues. Therefore, the necessary treatments for their restoration should also be performed.
Sometimes, the fracture may be dentoalveolar and the supporting bone around the tooth may be damaged. In such cases, the fractures are localized and limited, and reconstruction can be done without the need for general anesthesia.
Symptoms of Upper Jaw Fractures
- Looseness of the upper jaw skeleton
- Mouth being open in front
- Disruption of dental occlusion between the two jaws
- Pain
- Swelling
- Nasal bleeding
- Difficulty in chewing, eating, or speaking
- Loose, fractured, or missing teeth
- Improper alignment of teeth
- Cheek pain when opening the mouth
What is the Process of the Treatment of Upper Jaw Fractures?
The treatment of these fractures involves reduction followed by arch bar fixation for a period of 8 weeks, and then external fixation. In some limited cases, surgical intervention and open surgery are necessary, which will vary depending on the type of fracture and the extent of the injury.
An important consideration for these individuals is the evaluation and assessment of dental conditions following upper jaw or dentoalveolar fractures. In such cases, teeth are examined for luxation, vitality, and dental vascular and nerve involvement. If dental problems are detected, the need for preserving tooth functionality should be assessed, including root canal treatment if necessary, or in severe cases, the possibility of tooth extraction.
If the fracture of the upper jaw involves the lip or a portion of the tooth crown, dental aesthetic treatments such as repairing lip lacerations, veneers, or dental coatings should be considered as the final stage. It is recommended that dental issues be addressed after addressing jaw problems, fracture management, and jaw corrections.
If nasal bleeding is observed during the trauma and fracture, the patient should be aware that nasal bleeding is usually associated with sinus membrane or nasal mucosal laceration, which typically improves on its own within one to two weeks after surgery without the need for specific intervention. If it persists beyond this timeframe, it is advisable to consult a specialist maxillofacial surgeon.
Antibiotic therapy, antihistamine medications, nasal drops for airway clearance, and pain relievers are essential in these treatments.
A soft diet is recommended for up to 8 weeks following these fractures, after which the consumption of semi-solid and liquid foods is allowed. After 6 months, the patient can gradually return to a normal diet.
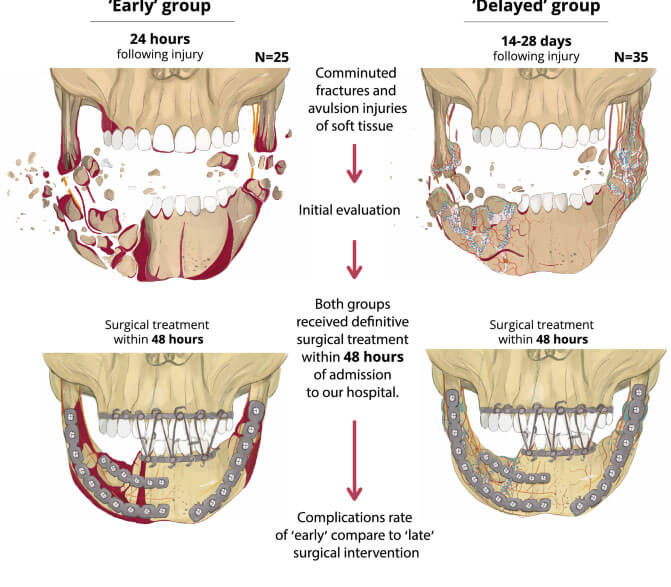
Treatment methods for maxillary (upper jaw) fractures include open reduction and closed reduction.
- Open Reduction
- Closed Reduction
- Combined Open and Closed Reduction
During this surgical procedure, jaw reduction, dental occlusion correction, and fixation with screws and plates are performed. In some cases, intermaxillary fixation (IMF) using wires and elastics may be required.
In this method, the mouth and teeth are usually closed using intraoral wires for up to 6 weeks. After fixation, the patient is regularly monitored and undergoes check-ups as determined by the maxillofacial surgeon. The duration of the closure varies from one to two months, depending on the fracture condition, as determined by the specialist. The patient follows specific feeding techniques for nourishment.
This approach combines both open and closed reduction methods, as described above.
Treatment of Facial and Jaw Fractures
If you have experienced sudden accidents, altercations, trauma, or injuries to the head, face, and neck, resulting in deformities or fractures in your face and jaw, you can visit our specialist maxillofacial surgeon for corrective measures.
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
- Saturdays: 14:00 to 20:00 - Punak clinic
- Sundays: 14:00 to 20:00 - Shariati clinic
- Mondays: 14:00 to 20:00 - Punak clinic
- Thursday: 14:00 to 20:00 - Saveh clinic
Postoperative Instructions for Jaw Fractures
- Take prescribed medications as instructed until the last dose.
- Rinse your mouth and teeth with chlorhexidine mouthwash twice a day for two weeks, and then continue using it once a night for one month.
- Use a soft toothbrush and brush all dental areas, including intraoral wires.
- The patient's diet should consist of fluids for approximately one month. If the patient's mouth is wired shut, fluids should be consumed using a syringe. If the mouth is open and not wired shut, limited intake can be done using a teaspoon. Rather than large volumes, frequent feeding should be emphasized.
- Consumption of protein-rich foods such as meat broth, rice water, and natural vitamins like fruit juice and pineapple juice is essential.
- Showering is allowed.
- While sleeping, the patient should sleep in a supine position and two pillows should be placed beside their face to prevent unintentional head movements to the sides.
- The head should be positioned at a 35-degree upward angle during sleep.
- It is normal to experience nasal bleeding within the first 48 hours.
- Nasal congestion and airway obstruction are common for approximately two weeks after the surgery and can be controlled with medication.
- After the operation, avoid any pressure or impact on the jaw and face. Special care is recommended for a minimum of 8 weeks following surgery.
Submental Fracture
Submental fracture, or condylar fracture, is the most common type of fracture among patients and mostly occurs in serious accidents or altercations.
Closed reduction (fixing the two jaws using arch bars) or open reduction (fixation with screws and plates) methods are used for the treatment of these fractures.
The treatment method in open surgery can be performed with intraoral or extraoral incisions. Dental occlusion should be established at the end of the treatment.
Complications of these types of fractures are usually significant. Complications such as temporomandibular joint dysfunction, functional disturbances, swallowing or speech difficulties, orthognathic problems, dental fractures and misalignments, numbness of the lip and chin, and lack of coordination during mouth opening and closing are the major sequelae after this injury.
Therefore, timely treatment and regular check-ups greatly assist in the patient’s recovery process.
- Mandibular fractures in edentulous individuals with severe atrophy
In these cases, after repositioning for fixation, thicker plates and plate reconstructions are used. The incision is made outside the mouth, and in many cases, due to the poor quality and quantity of the affected bone area, bone grafting (e.g., from the hip) is required for a more appropriate treatment.
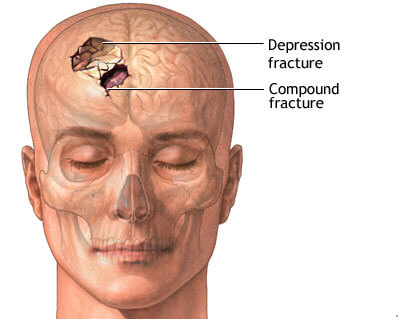
Frontal Bone Fracture
Severe head and frontal trauma can cause fractures in the frontal bone and floor of the sinuses.
The central part of the frontal bone is relatively weaker and thinner compared to the sides, and a severe impact to this area can result in inward displacement of the bone (depression). A considerable force is needed to fracture the frontal bone, but it is advisable to immediately consult a specialist maxillofacial surgeon after the incident.
Treatment is performed either immediately after the incident or one week later when swelling and inflammation have subsided. Frontal bone fractures are accompanied by complications such as swelling, pain, cerebrospinal fluid leakage, eye injuries, and sinus damage.
Any trauma or incident that leads to fractures in the facial and jaw area poses a risk to the individual’s functional and aesthetic aspects of life.
Zygomatic Fracture
The zygoma, also known as the cheekbone or malar bone, protrudes more (like the nasal bone) compared to other bones in the jaw and face. Therefore, in incidents that result in an impact to the jaw and face, the zygomatic bones are most susceptible to injury.
Symptoms such as pain, swelling, bruising, visual problems, double vision, nasal deformity, and intraoral bruises are consequences of zygomatic fractures, which can vary depending on the type of impact.
The treatment for zygomatic fractures is usually performed immediately after the incident or delayed by approximately one week by your maxillofacial surgeon to allow for the reduction of swelling and inflammation, ensuring better and more optimal treatment. In some cases, a fracture may result in a partial fissure on the zygoma, in which case your maxillofacial surgeon may choose not to perform surgery and provide specific instructions and care for natural healing and reconstruction over time.
In some cases, the fractures can be deep and extensive, shattering the bone into fragments. In such cases, your maxillofacial surgeon initiates repair and reconstruction through small incisions made internally and externally in the mouth, gaining access to the injured area. Subsequently, open reduction and internal fixation with screws and plates are performed.
During this period, it is important to be cautious and avoid any impact or pressure on the affected area, as the zygomatic bone may become dislocated from its position. Additionally, refrain from blowing your nose forcefully for a period of approximately two weeks to one month.
The screws used for bone fixation remain within the bone and do not need to be removed in the future. They are made of titanium and are compatible with the human body, unless your surgeon recommends their removal in the coming years. In that case, it is advisable to follow the surgeon’s opinion and instructions.
Approximately six months later, during the periodic check-ups, the surgeon prescribes a new imaging study to assess the precise deformities in this area. If deformities are observed in the CT scan, the following treatments are subsequently considered and performed:
- Osteotomy and re-fixation with screws and plates on the zygoma for repositioning.
- Facial implants (prostheses) for facial reconstruction.
- Bone grafts from the patient’s own bone tissue or allografts.
- Soft tissue correction using fat injection or fillers.
If the impact has affected the eye socket, it is likely to cause double vision or visual problems for the patient. In such cases, your maxillofacial surgeon advises consulting an ophthalmologist to address both bone corrections and visual issues.
For fractures of the orbital floor or eye socket, the repair and reconstruction of the damaged bone are usually performed through an incision in the eye socket and a brief incision inside the mouth simultaneously, ensuring precise and comprehensive access to the zygomatic bone.
- Zygomatic Arch Fracture
- ZMC Fracture
- Treatment methods for ZMC Fracture
Zigomatic arch fractures, as part of zygomatic fractures, can lead to facial sagging in front of the ear. Due to the impingement of the lower jawbone in this area, there may be limited mouth opening. This fracture can occur independently or in conjunction with other fractures.
In such cases, reduction of the zygomatic arch is performed, and in limited cases, internal fixation is also required. Following the surgery, physiotherapy is essential as per the maxillofacial surgeon’s instructions to restore normal mouth opening range. Avoid applying any pressure to the zygomatic and facial area, and sleeping on the side of the fractured face is strictly prohibited.
The zygomatic bone consists of four pillars. There is a type of fracture known as ZMC (Zygomaticomaxillary Complex) fracture, which occurs when all the pillars of this bone are broken or displaced due to trauma or an accident. The following symptoms can be mentioned for this fracture:
Eye globe deformity in the inferior and lateral area of the eye
Double vision and blurred vision
Enophthalmos (sunken eye)
Zygomatic arch depression
Nasal bleeding due to sinus membrane laceration
Numbness of the skin in the infraorbital, upper lip, lower eyelid, and upper jaw teeth area
Pain upon touching the eye globe and inside the mouth in the affected area
Periorbital ecchymosis (bruising around the eye) and intraoral mucosa
Hemorrhage or bleeding in the white of the eye
Inability to open the mouth due to zygomatic arch fracture
During the surgical procedure, incisions are made inside and outside the mouth to access the injured area. After reduction of the zygomatic arch, fixation with screws and plates is performed below the eye and around the eye, where it connects to the upper jaw. Reconstruction of the orbital floor is usually accompanied by various types of titanium mesh or prostheses.
Fractures of the Jaw and Face
In cases of nasal fractures, it is sometimes possible to perform cosmetic or deviation treatments simultaneously with fracture management. Contact us to receive consultation from a specialist in maxillofacial surgery (rhinoplasty specialist).
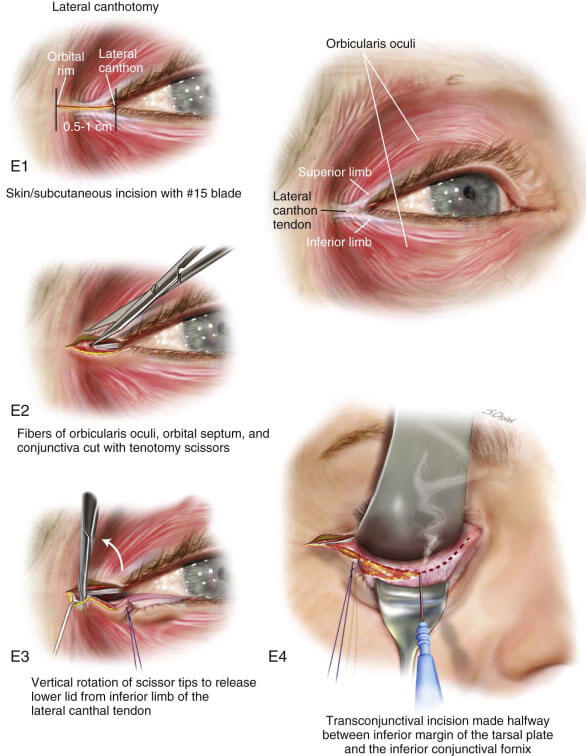
Orbital Fracture
An orbital fracture or eye socket fracture can occur independently or simultaneously with a zygomatic fracture. This type of fracture can result from impacts or accidents. After examining the clinical conditions and reviewing radiographs and CT scans, the maxillofacial surgeon may instruct a consultation with an ophthalmologist regarding eye health if he diagnoses orbital fracture.
For the treatment of this fracture, incisions are made inside the conjunctiva for orbital floor reconstruction, and if necessary, cutaneous incisions are also made.
Pain, swelling, bruising, subconjunctival hemorrhage, pupil position abnormalities, eye protrusion or enophthalmos, limited eye movement, paresthesia, or tingling sensation in the area under the eye and lower eyelid, blurred vision, and other signs are manifestations that the patient may experience following this fracture.

Nasal Fracture
After an incident resulting in a severe blow to the nose and a nasal fracture, it is advisable to immediately seek treatment from a maxillofacial surgeon. The patient realizes a nasal fracture following the incident, due to pain, swelling, and changes in the shape of the his nose.
Following the fracture and after obtaining the prescribed radiographs, your surgeon initiates treatment. Closed reduction is performed by the maxillofacial surgeon and then fixed using external and internal splints.
Approximately 3 to 4 days after treatment, the internal nasal splints are removed. Approximately ten days later, the external splint is removed, and ultimately monthly check-ups are recommended for up to six months.
[read more]
The entire process and type of treatment depend on the type of injury and impact, and naturally, different individuals receive different treatment plans. After approximately six months, if the surgeon observes deviation, asymmetry, or tilting of the nasal tip, further imaging is prescribed for a more accurate assessment, and if necessary, cosmetic surgical treatment plans are discussed. The following are signs of a nasal fracture:
Bleeding, decreased sense of smell, congestion, respiratory problems, airway obstruction, etc., which gradually diminish after the operation.
[/read]
Facial Fracture in Children
Sometimes, children are affected by facial fractures as a result of an accident. It is essential to consider the process of facial skeletal growth in these patients; therefore, treatments in such cases mostly involve closed reduction methods, and if necessary, open reduction methods are used with minimal incisions.
In these patients, very thin and absorbable plates are used for bone reconstruction. A notable and helpful aspect among pediatric patients is that the healing process occurs relatively faster compared to adults.
If the treatment is done using a closed reduction method, the use of splints sometimes aids the treatment. In such cases, dental impressions are taken, and a device called a splint is made, which is then fixed to both jaws after reduction, eliminating the need for screws and plates.
A significant consideration in fractures of the upper and lower jaw in these patients is attention to the fractures and repositioning of deciduous teeth and evaluation of the possibility of damage to permanent tooth germs. In mandibular fractures in children, due to the importance of the growth center in the mandible, special attention should be given to the growth of the mandibular symphysis, and the use of elastics by orthodontic colleagues may be necessary after surgical treatment.
